Keratoconus
Keratoconus is characterized by the thinning of the cornea and irregularities of the cornea’s surface
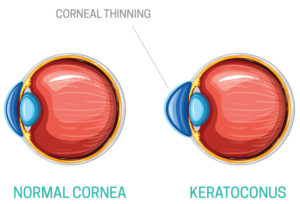 The cornea is the clear, outer layer at the front of your eye. The middle layer is the thickest part of the cornea, mostly made up of water and a protein called collagen. Collagen makes the cornea strong and flexible, and helps keep its regular, round shape. This healthy cornea focuses light so you can see clearly. With keratoconus, the cornea thins and bulges into an irregular cone shape, resulting in vision loss.
The cornea is the clear, outer layer at the front of your eye. The middle layer is the thickest part of the cornea, mostly made up of water and a protein called collagen. Collagen makes the cornea strong and flexible, and helps keep its regular, round shape. This healthy cornea focuses light so you can see clearly. With keratoconus, the cornea thins and bulges into an irregular cone shape, resulting in vision loss.
Keratoconus generally begins at puberty and progresses into the mid-30s. There is no way to predict how quickly the disease will progress, or if it will progress at all. Keratoconus typically affects both eyes, with one being more severely affected than the other.
Risk factors for keratoconus?
The following may increase the risk of developing keratoconus:
- Genetics. Patients with a family history of keratoconus or with certain systemic disorders, such as Down syndrome, are at a higher risk of developing keratoconus.
- Chronic eye inflammation. Constant inflammation from allergies or irritants can contribute to the destruction of corneal tissue that may result in developing keratoconus.
- Eye rubbing. Chronic eye rubbing is associated with developing keratoconus. It may also be a risk factor for disease progression.
- Age. Keratoconus is often discovered in the teenage years. Generally, young patients with advanced keratoconus are more likely to need some form of surgical intervention as the disease progresses.
What are the symptoms of keratoconus?
Many keratoconus patients are unaware they have the disease. The earliest symptom is a slight blurring of vision or progressively poor vision that is not easily corrected.
Other symptoms of keratoconus include:
- Glare and halos around lights
- Difficulty seeing at night
- Eye irritation or headaches associated with eye pain
- Increased sensitivity to bright light
- Sudden worsening or clouding of vision
How is keratoconus diagnosed?
In addition to a complete medical history and eye exam, your eye care professional may perform the following tests to diagnose keratoconus:
- Corneal topography. This is the most accurate way to diagnose early keratoconus and follow its progression. A computerized image is taken that creates a map of the curve of the cornea.
- Slit-lamp exam. This examination of the cornea can help detect abnormalities in the outer and middle layers of the cornea.
- Pachymetry. This test is used to measure the thinnest areas of the cornea.

